Advanced information
Advanced information:
Human in vitro fertilization (pdf)

Advanced information
Human in vitro fertilization
The 2010 Nobel Prize in Physiology or Medicine is awarded to Dr. Robert G. Edwards for the development of human in vitro fertilization (IVF), a medical advance that represents a paradigm shift in the treatment of many types of infertility. The inability to conceive a child is a reproductive defect that afflicts more than 10% of all couples worldwide. During the 1950s, Edwards came to realize the potential of IVF as a treatment for this medical condition. What inspired him to take on this challenge was his research on how hormones control critical ovarian functions in mice, such as oocyte maturation and ovulation. By a brilliant combination of basic and applied medical research, Edwards overcame one technical hurdle after another in his persistance to discover a method that would help to alleviate infertility. He was the first to show that human oocytes could undergo in vitro maturation, as well as fertilization in vitro. He was also the first to show that in vitro fertilized human oocytes could give rise to early stage embryos and blastocysts. All of Edwards’ accomplishments came together at 11.47 PM, on July 25 1978 with the birth of Louise Joy Brown, the worlds’ first child conceived through IVF. Dr. Robert G. Edwards’ research has completely transformed the field of reproductive medicine and today close to 4 million babies have been born thanks to the discovery of human IVF.
Introduction
Infertility is a widespread condition known to affect more than 10% of all couples worldwide. It is regarded as psychologically stressful by most individuals and can lead to depression, social isolation and a lower quality of life1. Historically, little medical help has been available to infertile individuals, who were therefore forced to risk their health and even lives, by taking part in more or less obscure infertility-treatment practices. Female infertility is often due to damage to the Fallopian tubes, obstructing a contact between the egg and the sperm (Fig. 1), whereas male infertility is linked to impaired sperm quantity and quality.
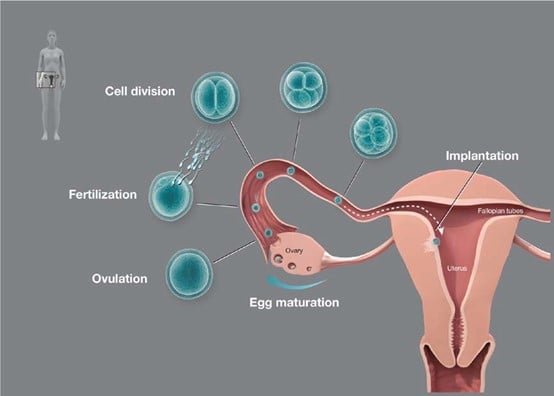
Female gametes are stored in the ovaries as separate follicles, i.e. each follicle contains one germ cell surrounded by one or several layers of granulosa cells. Humans (as well as other mammals) are born with a defined pool of primordial oocytes which are arrested at the dictyate stage of meiosis I. In sexually mature women, follicle stimulating hormone signaling and other factors stimulate the maturation of individual follicles on a monthly basis, generating primary and secondary follicles. In response to a rapidly increased concentration of luteneising hromone, a cascade of events are initiated, including further oocyte growth and meiotic resumption. Reactivation of meiosis completes the first meiotic chromosome segregation event and results in one set of chromosomes that become arrested at the metaphase stage of meiosis II, and a second set of chromosomes that are discarded (the first polar body). Following this, the mature follicle ruptures and ovulation ensues, a process in which the egg is is released from the ovary into the fallopian tubes (the oviduct). Sperm, entering from the uterus, will move towards the released egg from the opposite end of the fallopian tubes. Successful penetration of a single sperm through the egg coat will initate a set of sperm-egg interaction events that relieves the meiosis II arrest of the egg. This results in the formation of two haploid sets of chromosomes, one set that will fuse with the haploid set of chromosomes contributed by the sperm, and a second set that is discarded (the second polar body). The fertilization process give rise to an embryo that undergoes a number of cell divisions while being transported through the fallopian tubes towards the uterus. Once in the uterus, the embryo (now at the blastula stage) will implant into the wall of the uterine lining, called the endometrium. Further embryo development will then take place at this location. © The Nobel Committee for Physiology or Medicine. Ill. Mattias Karlén
Early research on in vitro fertilization in mammals
The in vitro fertilization process was first studied in non-mammalian species, for example marine animals, where the fertilization process most often takes place outside the body in an aquatic environment. The first observation of sperm penetration into an egg was reported in Ascaris by Nelson in 1851 and subsequent studies in non-mammalian species have provided many important details of the fertilization process.
Gregory Pincus, at the Worcester Foundation for Experimental Biology in the US, described in 1935 the first experimental conditions that allowed mammalian oocytes (from rabbit) to mature in vitro, reaching the metaphase stage of meiosis II2. Min Chueh Chang, at the same research institute as Pincus, showed in 1959 that in vitro-matured rabbit oocytes could be fertilized in vitro and also give rise to viable embryos3. Furthermore, when these embryos where transferred back to adult females, they gave rise to viable offspring3. Chang’s findings represented a significant advancement, however, a caveat with these studies was the necessity to pre-incubate sperm in the uterus of a pregnant female prior to attempting to fertilize the oocytes3. The reason why Chang did not use strict in vitro conditions in these experiments was a general belief at this time that sperm required activation (capacitation) in vivo to contribute to fertilization in vitro4, 5. Ryuzo Yanagimachi and Min Chueh Chang in 1963 showed that this dogma was incorrect, when they identified experimental in vitro conditions through which spermatozoa (from hamster) without prior in vivo activation, could fertilize oocytes and give rise to 2-cell stage embryos6.
Human in vitro fertilization – a monumental challenge
In the first part of the 20th century, researchers studying reproduction began to discuss the possibility of defining conditions that would allow human oocytes to be fertilized in vitro. The immense complexity of the fertilization process was a challenge and despite advances in animal reproductive research, no progress had yet been made regarding IVF of human oocytes in the early 1960s. Several technical advances and discoveries would be required before successful human IVF could be achieved; the ability to control the oocyte maturation process, the ability to retrieve oocytes at a developmental stage suitable for IVF, the ability to activate sperm in vitro, the ability to define conditions that would promote fertilization as well as early embryo development in vitro and finally, a method through which early embryos could be transfered back to the uterus of the mother.
Robert G. Edwards, working at the National Institute for Medical Research in London in the late 1950s, was committed to develop a method that would alleviate human infertility. Edwards had an exceptionally broad knowledge of the fertilization process, gained through many years of basic research on animal reproductive physiology, and he was therefore well prepared for this challenge7-14. The first problem that he had to solve was to find a method that provided access to mature oocytes suitable for IVF. His first choice was to try to identify conditions that would promote maturation of human oocytes in vitro. He knew from the work of Pincus that mammalian oocytes seemed to require only a few hours of cultivation in vitro before they assumed meiotic maturation2. Starting from immature human oocytes that had been released from ovarian tissues, Edwards tried for several years to find in vitro conditions that would activate these dormant oocytes. Edwards’ work was rewarded in 1965 when he discovered that human oocytes, in contrast to the prevailing dogma, required 24 hours of incubation in vitro, before they would initiate their maturation process15, 16. Importantly, the in vitro maturation method also provided oocytes at a late developmental stage (the metaphase stage of meiosis II), suitable for IVF. Edwards’ next research challenge was to find conditions that would promote fertilization of oocytes in vitro. Barry D. Bavister, a graduate student of Edwards at Cambridge University, had recently identified buffer conditions to support in vitro activation of hamster sperm17. Edwards, using these buffer conditions, showed in 1969 that activated human spermatozoa could promote fertilization of in vitro matured oocytes18. This result represents an important discovery and a milestone in reproductive research as it opened the way for the development of a method to treat infertility.
The Breakthrough
Edwards’ research on in vitro maturation of human oocytes, however, had given him a crucial insight. He had found that while human oocytes that had matured in vitro could be fertilized, they failed to progress beyond the 2-cell stage. This failure could be attributed to the lengthy periods that in vitro matured oocytes had to spend outside the body. Edwards now instead decided to try to use oocytes that had completed their maturation process in vivo. Edwards postulated that if mature human oocytes could be retrieved from the ovary prior to the onset of ovulation, these oocytes would be more competent to undergo IVF and early embryo development (Fig. 1 and Fig. 2).
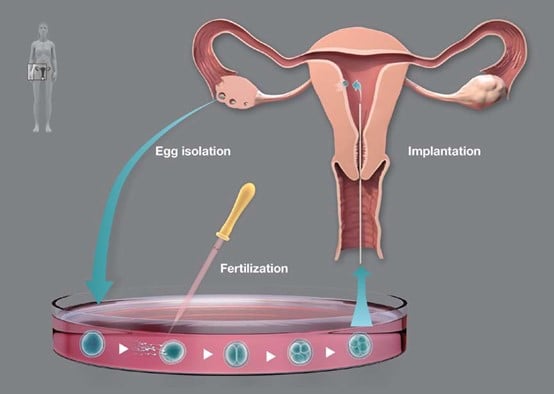
Oocytes arrested at the metaphase stage of meiosis II are retrieved prior to ovulation from the ovary by laparoscopy. The oocytes are placed in a culture dish with medium and mixed with sperm. The medium condition promotes sperm activation in vitro, a necessary requirement for the fertilization process. The egg-sperm interactions relieve the meiosis II arrest of the egg. This results in the formation of two haploid sets of chromosomes, one set that will fuse with the haploid set of chromosomes contributed by the sperm, and a second that is discarded (the second polar body). The fertilization process results in the formation of an embryo that undergoes a number of cell divisions in vitro. The embryo is transferred back to the uterus at the eight-cell stage (2.5 days after onset of fertilization) using a thin needle. The embryo will divide further in the uterus until it reaches the blastula stage and thereafter implant into the wall of the uterine lining, the endometrium. Further embryo development will take place at this location. © The Nobel Committee for Physiology or Medicine. Ill. Mattias Karlén
Edwards’ new approach arose from his previous work on the reproductive biology of the mouse. He had shown that initiation of meiotic maturation of oocytes could be controlled by externally provided gonadotrophins, i.e. hormones that mimicked the function of the intrinsically acting hormone (luteneising hormone)12, 13. He also knew that it took an equally long time in vitro and in vivo to mature mouse oocytes to the metaphase II stage of meiosis, and from his in vitro studies of human oocytes, also the timing of the meiotic maturation process in humans was known. However, Edwards’ (now at Cambridge University) new strategy raised an important technical problem; no method known to him could retrieve a sufficient number of human oocytes from the ovary at the correct stage of development. In the late 1960s, access to human oocytes required the surgical removal of a small part of the ovary from infertile women, an approach not suitable for IVF. Reading a scientific article written by Dr. Patrick C. Steptoe19, Edwards became aware of a new method called laparoscopy. Laparoscopy allowed the human female reproductive tract to be visualized by a fiber-optic endoscope inserted through an incision near the navel. Steptoe (working at the Oldham and District General Hospital) was a skilled surgeon and obstetrician, who had introduced and developed the use of laparoscopy in England and shown that it was possible to aspirate oocytes from the ovary. Edwards immediately realized that this method could be used to retrieve oocytes at the metaphase stage of meiosis II from the ovary during a suitable period of the menstrual cycle. Edwards therefore contacted Steptoe and they showed in 1970 that mature preovulatory oocytes at the metaphase II stage of meiosis could indeed be retrieved from infertile women after priming ovaries with gonadotrophins20.
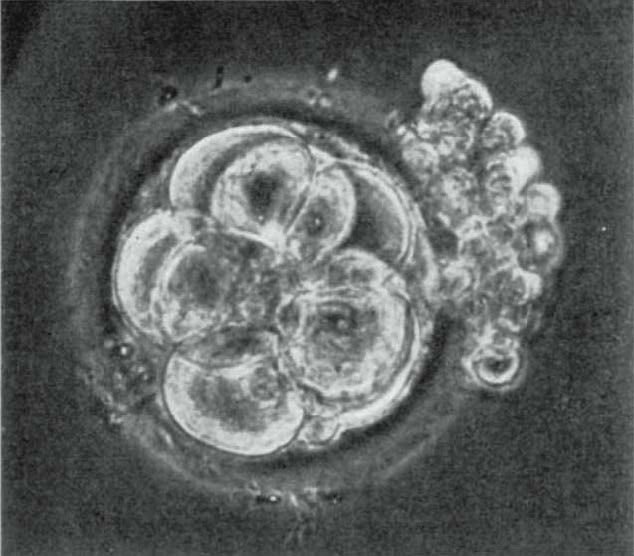
Edwards subsequently reported that IVF of preovulatory oocytes using in vitro activated sperm could give rise to 8-cell stage human embryos21. This was a seminal finding in two respects, it was the first time that in vitro activated sperm had been shown to be capable of contributing to embryo development beyond the 2-cell stage in a mammalian system and it was the first time human embryos had been shown to undergo cell divisions in vitro (Fig. 3). Following this, he then showed in 1971 that human oocytes fertilized in vitro could undergo further cleavage generating 16-cell stage embryos and forming blastocysts in vitro22. The series of discoveries made by Edwards during 1969-1971 represent important milestones in IVF research and set the stage for the next phase to come.
In the early 1970s, Edwards and Steptoe started to transfer the early embryos that resulted from IVF back into women. After more than one hundred attempts that all led to short-lived pregnancies, they realized that the hormone treatments given to women to induce oocyte maturation disturbed implantation of the embryo in the uterus, resulting in spontaneous abortions. Finally, after a change in the hormone treatment protocol, the first successful pregnancy was achieved in 197623. Unfortunately, the embryo had implanted ectopically in the Fallopian tube and the pregnancy had to be terminated. Edwards and Steptoe then decided to abandon the ovarian stimulation protocol altogether and instead rely on the natural menstrual cycle of the patients, although this meant that they would have access to only one egg per cycle. Based on the concentration of luteinizing hormones in the urine of the women, they could predict when the maturing oocyte would reach the metaphase stage of meiosis II in vivo. They hoped that they then would be able to retrieve the egg by laparoscopy before ovulation occurred. Steptoe and Edwards succeeded in their efforts and in 1978 they made the historic announcement that a normal, fit and healthy baby, Louise Joy Brown, had been born through successful IVF of a human oocytes24, 25. Edwards’ long-term vision and persistence had finally come to fruition, opening up a new era in the treatment of infertility (Fig. 4).
Further developments of IVF
Following the birth of Louise Brown, Edwards and Steptoe founded an infertility clinic at Bourn Hall, in Cambridge, UK, where they continued to develop the IVF method. The second and third child in the world conceived through IVF was born at Bourn Hall Clinic26. Bourn Hall rapidly became a center for IVF research and successful modifications were made to the experimental protocols used for hormonal ovarian stimulation and embryo cultivation at Bourn Hall Clinic27, 28, resulting in 139 births by 1983 and 1,000 births by 1986. Rapid advances in IVF methodology now also began to take place outside the Bourn Hall Clinic and by 1986 about 1,000 additional births had been reported in other countries. Today, close to 4 million babies have been born worldwide as a result of IVF29. A large majority of infertile women can now be helped to conceive a baby as a result of IVF30. The first generation of children conceived through IVF, including Louise Joy Brown, are now of reproductive age. Several of them have had children of their own, without the need for IVF.
Further medical developments
Edwards’ seminal achievements attracted many other researchers to the field of reproductive medicine, resulting in rapid technical development. The laparoscopic recovery of oocytes was replaced by a vaginal ultrasound-guided oocyte recovery method31 and cryopreservation of surplus human embryos was introduced32. Successful IVF of in vitro matured human oocytes was reported in 199433, a method important to women that are sensitive to ovarian hormone stimulation protocols and to women that risk losing their ovarian pool of oocytes due to treatment of cancer. The development of intra-cytoplasmic sperm injection (ICSI), in which single sperm are microinjected into the cytoplasm of the mature egg, represented a technological breakthrough, making it possible to also to treat many categories of male infertility34.
Edwards’ work on human embryonic cells and blastocysts21, 22 was also instrumental for later work that resulted in the derivation of human embryonic stem cells35, which has been important for our understanding of cellular differentiation, and may become important in regenerative medicine in the future. The IVF method has also been instrumental for the development of preimplantation genetic diagnostics (PGD). PGD is a procedure performed in vitro on in vitro fertilized early embryo cells to reduce the risk that parents transmit a severe genetic disorder or a chromosomal abnormality to their children36, 37.
Health status of offspring conceived through in vitro fertilization
Children born after IVF are in general as healthy as children born after natural conception according to several long-term follow-up studies38-42. There is, however, a higher frequency of multiple births associated with IVF treatments compared to normal pregnancies39-42. This is largely due to the practice at some infertility clinics of transferring two or more embryos back into the mother. Multiple births are associated with an increased risk for preterm birth, low birth weight and cesarean sections, factors that could give rise to perinatal and postnatal health problems. Many European countries have introduced mandatory or voluntarily regulatory procedures that insist on single embryo transfers, which have dramatically reduced the incidence of multiple births after IVF38-42. Despite the introduction of the single embryo transfer policy, a two-fold increased risk for preterm birth for women undergoing IVF treatment remains42. This could be explained by the older age of these women or by factors related to the underlying cause of their infertility. It has been shown that the use of IVF slightly increases the frequency of two imprinting disorders, Beckwith-Wiedemann Syndrome (BWS) and Angelman Syndrome (AS), although the absolute risk is still small as both diseases are very rare in the general population43. Meta-analyses of controlled studies have reported an increased risk of major malformations (defined as a condition that causes functional impairment or requires surgical correction) in children conceived through IVF, however, the underlying studies lack appropriate control groups and have significant methodological limitations39, 44.
Ethical considerations
Edwards realized from the onset that IVF research would raise many important ethical concerns that had to be addressed. He wrote, together with the lawyer David Sharpe, a visionary key paper that initiated a debate on many of the complicated issues related to reproductive medicine that lay ahead45. They argued that research on human germ cells and embryos should be conducted under strict ethical guidelines. Edwards himself acted forcefully on these issues, as he ensured that an Ethics Committee for IVF was created at Bourn Hall Clinic. Since 1978 Edwards has taken a very active part in ethical discussions on many different aspects of human reproductive research. Despite Edwards’ persistent attention to ethical and safety questions, his work on IVF initially met with strong opposition from religious leaders saying that this was morally wrong, from government officials who felt it was more important to limit fertility than to treat infertility and from scientific colleagues whose criticism was based on embryo safety issues, the latter aspect being one of the reasons why the Medical Research Council in the UK rejected an application submitted by Edwards and Steptoe in 1971 for IVF research46-48. In retrospect, it is amazing that Edwards not only was able to respond to the continued criticism of IVF, but that he also remained so persistent and unperturbed in fulfilling his scientific vision.
Conclusions
Robert G. Edwards has developed a method to treat human infertility. This discovery represents a monumental medical advance that can truly be said to confer the “greatest benefit to mankind”. Human IVF has radically changed the field of reproductive medicine. Today, 2-3% of all newborns in many countries are conceived with the help of IVF and many individuals that turn to an infertility clinic can be helped. IVF has also opened up new ways to treat many forms of male infertility. The development of IVF recognized by this year’s Nobel Prize in Physiology or Medicine has touched the life of millions of infertile people, giving them an opportunity to have children.
Christer Höög
Professor of Cell Biology, Karolinska Institutet, Stockholm
Member of the Nobel Assembly
Acknowledgements
I am grateful to Mattias Karlén for designing the figures and to Adam Smith for helpful comments on the text.
References
1. Johansson, M., Adolfsson, A., Berg, M., Frances, J., Hogström. L., Janson, P. O., Sogn, J. and Hellström, A. L. (2009) Quality of life for couples 4-5.5 years after unsuccessful IVF treatment. Acta Obstet. Gynecol. Scand. 88:291-300.
2. Pincus, G. and Enzmann, E. V. (1935) The comparative behavior of mammalian eggs in vivo and in vitro: I. The activation of ovarian eggs. J. Exp. Med. 62:665-675.
3. Chang, M. C. (1959) Fertilization of rabbit ova in vitro. Nature 184:466-467.
4. Chang, M. C. (1951) Fertilizing capacity of spermatozoa deposited into the Fallopian tubes. Nature 168:697-698.
5. Austin, C. R. (1951) Observation on the penetration of sperm into the mammalian egg. Austr. J. Sci. Res. (Serie B) 4:581-596.
6. Yanagimachi, R. and Chang, M. C. (1963) Fertilization of hamster eggs in vitro. 200:281-282.
7. Edwards, R. G (1954) Colchicine-induced heteroploidy in early mouse embryos. Nature 174:267-277.
8. Edwards, R. G. (1955) Selective fertilization following the use of sperm mixtures in the mouse. Nature 175:215-216.
9. Edwards, R. G. and Sirlin J. L. (1956) Labeled pronuclei in mouse eggs fertilized by labeled sperm. Nature 177:429.
10. Sirlin J. L. and Edwards, R. G. (1957) Duration of spermatogenesis in the mouse. Nature 180:1138-1139.
11. Fowler, R. E. and Edwards, R. G. (1957) Induction of superovulation and pregnancy in mature mice by gonadotrophins. J. Endocrin. 15:374-384.
12. Edwards, R. G. and Fowler R. E. (1958) The experimental induction of superfoetation in the mouse. J. Endocrin. 17:223-236.
13. Edwards, R. G. and Gates A. H. (1959) Timing of the stages of the maturation divisions, ovulation, fertilization and the first cleavage of eggs of adult mice treated with gonadotrophins. J. Endocrin. 18:292-304.
14. Edwards R. G. and Sirlin J. L. (1959) Fate of spermatozoa penetrating into the tissues of the fallopian tube. Nature 183:1744-1745.
15. Edwards, R. G. (1965) Maturation in vitro of mouse, sheep, cow, pig, rhesus monkey and human ovarian oocytes. Nature 208:349-351.
16. Edwards, R. G. (1965) Maturation in vitro of human ovarian oocytes. The Lancet 2:926-929.
17. Bavister, B. D. (1969) Environmental factors important for in vitro fertilization in the hamster. J. Reprod. Fertil. 18:544-545.
18. Edwards, R. G., Bavister, B. D. and Steptoe, P. C. (1969) Early stages of fertilization in vitro of human oocytes matured in vitro. Nature 221:632-635.
19. Steptoe, P. C. (1968) Laparoscopy and ovulation. Lancet ii, 913.
20. Steptoe, P. C. and Edwards, R. G. (1970) Laparoscopic recovery of preovulatory human oocytes after priming of ovaries with gonadotrophins. Lancet 1:683-689.
21. Edwards, R. G., Steptoe, P. C. and Purdy, J. M. (1970) Fertilization and cleavage in vitro of preovulator human oocytes. Nature 227:1307-1309.
22. Steptoe, P. C., Edwards, R. G. and Purdy, J. M. (1971) Human blastocysts grown in culture. Nature 229:132-133.
23. Steptoe, P. C. and Edwards, R. G. (1976) Reimplantation of a human embryo with subsequent tubal pregnancy. Lancet 1:880-882.
24. Steptoe, P. C. and Edwards, R. G. (1978) Birth after the reimplantation of a human embryo. Lancet 2:366.
25. http://www.youtube.com/watch?v=pqu8Y4XGFK4
26 Edwards, R. G., Steptoe, P. C. and Purdy, J. M. (1980) Establishing full-term human pregnancies using cleaving embryos grown in vitro. Br. J. Obstet. Gynaecol., 87: 737-756.
27. Edwards, R. G. and Steptoe, P. C. (1983) Current status of in-vitro fertilization and implantation of human embryos. The Lancet 2:1265-1269.
28. Steptoe, P. C., Edwards, R. G. and Walters, D. E. (1986) Observations on 767 clinical pregnancies and 500 births after human in-vitro fertilization. Hum. Reprod. 1:89-94.
29. Data presented at the 2010 Annual Conference of the European Society of Human Reproduction and Embryology in Rome.
30. Malizia, B. A., Hacker, M. R. and Penzias A. S. (2009) Cumulative live-birth rates after in vitro fertilization. N. Engl. J. Med. 360:236-243.
31. Wikland, M., Hamberger, L., and Enk, L. (1985) Transvesical and transvaginal approaches for aspiration of follicles by use of ultrasound. III World Congress of in vitro fertilization and embryo transfer. Helsinki 1984. Ann NY Acad Sci 442:182-194.
32. Trounson, A. and Mohr, L. (1983) Human pregnancy following cryopreservation thawing and transfer of an eight-cell embryo. Nature 305:707-709.
33. Trounson, A., Wood, C. and Kausche, A. (1994) In vitro maturation and the fertilization and developmental competence of oocytes recovered from untreated polycystic ovarian patients. Fertil. Steril. 62:353-362.
34. Palermo, G., Joris, H., Derde, M. P., Camus, M., Devroey, P., Van Steirteghem A., C. (1993) Sperm characterization and outcome of human assisted fertilization by subzonal insemination and intracytoplasmic sperm injection. Fertil. Steril. 59:826-835.
35. Thomson, J. A., Itskovitz-Eldor, J., Shapiro, S. S., Waknitz, M. A., Swiergiel, J. J., Marshall, V. S. and Jones, J. M. (1998) Embryonic stem cell lines derived from human blastocysts. Science 282:1145-1147.
36. Handyside, A., Kontogianni, E. H., Hardy, K. and Winston, R. M. (1990) Pregnancies from biopsied human preimplantation embryos sexed by Y-specific DNA amplification. Nature 344:768-770.
37. The Practice Committees of the Society for Assisted Reproductive Medicine and the American Society for Reproductive Medicine. (2007) Preimplantation genetic testing: a Practice Committee opinion. Fertil. Steril. 88:1497-1504.
38. International Committee for monitoring assisted reproductive technology (ICMART): de Mouzon, J., Lancaster, P., Nygren, K. G., Sullivan, E., Zegers-Hochschild, F., Mansour, R., Ishihara, O. and Adamson, D. (2009). World collaborative report on assisted reproductive technology, 2002. Hum. Reprod. 24:2310-2320.
39. Ludwig, A. K., Sutcliffe, A. G., Diedrich, K. and Ludwig, M. (2006) Post-neonatal health and development of children born after assisted reproduction: A systematic review of controlled studies. Eur. J. Obstetrics & Gynecology and Reprod. Biol. 127:3-25.
40. Basatemur, E. and Sutcliffe, A. (2008) Follow-up of children born after ART. Placenta 29:S135-S140.
41. Nygren, K. G., Finnström, O., Källen, B. and Otterblad Olausson, P. (2007) Population-based Swedish studies of outcomes after in vitro fertilization. Acta Obstetricia et Gynecologica 86:774-782.
42. McDonald, S. D., Han, Z., Mulla, S., Murphy, K. E., Beyene, J., Ohlsson, A; Knowledge Synthesis Group (2009) Preterm birth and low birth weight among in vitro fertilization singletons: a systematic review and meta-analyses. 146:138-148.
43. Amor, D. J. and Halliday, J. (2008) A review of known imprinting syndromes and their association with assisted reproduction technologies. Hum. Reprod. 23:2826-2834.
44. Rimm, A. A., Katayama, A. C., Diaz, M. and Katayama, K. P. (2004) A meta-analysis of controlled studies comparing major malformation rates in IVF and ICSI infants with naturally conceived children. J. Assisted Reprod. Genet. 21:437-443.
45. Edwards, R. G. and Sharpe, D. J. (1971) Social values and research in human embryology. Nature 231:87-91.
46. Edwards, R. G. and Steptoe, P. C. (1980) A matter of life. London: Hutchinson.
47. Edwards, R. G. (2001) The bumpy road to human in vitro fertilization. Nature Medicine 7:1091-1094.
48. Johnson, M. H., Franklin, S. B., Cottingham, M. and Hopwood N. (2010) Why the Medical Research Council refused Robert Edwards and Patrick Steptoe support for research on human conception in 1971. Hum. Reprod. 25:2157-2174.
© The Nobel Committee for Physiology or Medicine 2010
Nobel Prizes and laureates
See them all presented here.