Unleashing the power of the immune system to fight cancer
For more than a century, scientists searched in vain for way to unleash the natural power of the immune system to fight cancer. Their dream is now a reality after two laureates found methods that block the brakes of the immune system and allow it to wage war against tumours. Their work has revolutionised cancer care, to give survivors “the gift of life”.
Just one year after being diagnosed with tonsil cancer, Tomas Dahl received the news every patient dreads; nothing more could be done to save his life after conventional cancer treatments had failed. “I had a few months left to live. I explained to my kids that I would not make it,” he said.
However, a new treatment cancer therapy born out of research by the 2018 medicine laureates James Allison and Tasuku Honjo, offered him fresh hope. Dahl received a type of immunotherapy drug that uses the power of the body’s own immune system to control, and eliminate cancer, to give him “the gift of life”.
Today, immunotherapy is a fourth pillar of cancer treatment and is used alongside radiation, chemotherapy and surgery. By orchestrating the immune system in the right way, it has proved possible to control or eliminate cancer in tens of thousands of patients.
Redefining treatment and saving lives
Sharon Belvin was one of the first patients to benefit from an immune checkpoint inhibitor drug which is one form of immunotherapy widely available today. At the age of 22, she was looking forward to getting married, but was instead diagnosed with a type of skin cancer called metastatic melanoma that had spread to her lungs, lymph nodes and brain. “Every single conventional therapy for melanoma was not very effective. It was a death sentence at the time,” she said.
Belvin was offered the opportunity to participate in a clinical trial for immunotherapy and received a checkpoint inhibitor called ipilimumab, which was invented by Allison. It was the first treatment of any type with the ability to offer the hope of survival for patients with metastatic melanoma.
“It worked textbook,” she said. Belvin’s tumours grew smaller until there was no evidence of cancer after one round of treatment. Without him [Allison], without my oncologist, my kids wouldn’t be here. My husband wouldn’t have a wife,” Belvin said.
Allison received a phone call from Belvin’s doctor suggesting an impromptu meeting with her – it was to have a profound impact on him. Despite knowing his work had incredible potential, the clinical trials of his checkpoint inhibitor drug were mostly numbers to him at first.
“I went over to the outpatient clinic and walked into this room with her doctor and she and her husband, and her parents. I suppose it was a life-changing moment,” Allison said. The two both cried when Belvin told him she was tumour-free and they kept in touch, with Belvin sharing news about the birth of her two children. “There are no words to describe what it feels like […] when you have handed someone back their life,” Belvin said.
Immune checkpoint therapy has fundamentally changed the outcome for certain groups of patients with advanced cancer, including Belvin and Dahl, who were among several cancer patients who joined the two Nobel Prize laureates in Stockholm, Sweden in December 2018 to celebrate their achievement.

“There simply aren’t words to express the gratitude I feel. I would not be here today if it wasn’t for you and your discovery,” Dahl told the laureates at the emotionally-charged event.
Today checkpoint inhibitors have become a standard treatment for a growing list of cancers, and have proven effective for treating small cell lung cancer and non-small cell lung cancer, bladder cancer, kidney cancer, stomach cancer, liver cancer, head and neck cancers, lymphoma and melanoma.
“Meeting the people who have benefitted from our research is the real prize for me,” said Allison. “When I meet patients who tell me: ‘You saved my life,’ it is an unforgettable moment,” Honjo added.
Blocking the brakes of the immune system
Allison said he wanted to “do something about cancer,” having witnessed the “ravages of conventional therapies” before losing his mother and other family members to the disease, but he did not initially expect his research on the workings of the immune system to lead to a new cancer treatment.
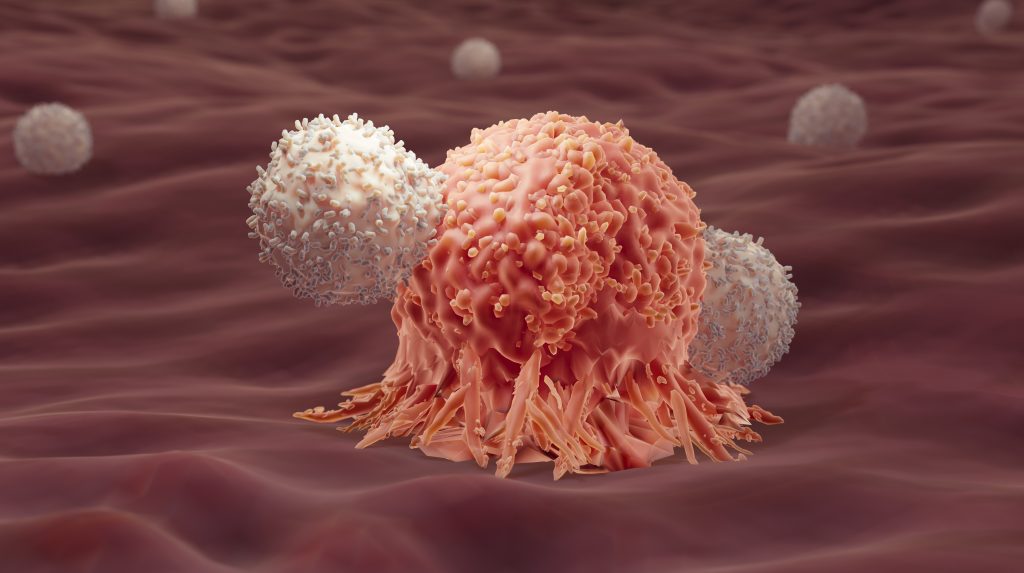
Both Allison and Honjo set out to understand how a type of white blood cell called T cells work. T cells can detect invading bacteria, viruses and other dangers such as cancer before multiplying and recruiting other elements of the immune system to join the fight. “They can recognise almost anything that nature throws at you,” Allison explains.
T cells can identify dangers by using a protein on their surface called the T cell receptor that binds to invaders and triggers the immune system to fight them. Additional proteins acting as T-cell accelerators are also required to trigger a full-blown immune response. During the 1990s, Allison studied a protein on the surface of T cells called CTLA-4. He was one of several scientists who observed that CTLA-4 functions as a brake on T cells, preventing them from attacking invaders, and thus also regulating the immune cells to avoid them attacking our own tissues. This intricate balance between accelerators and brakes is essential for tight control of the immune system.
While other research teams wanted to see whether this braking mechanism could be used to treat autoimmune diseases, Allison had an entirely different approach. “One of the ideas I had was that maybe the reason that the immune system isn’t so good at attacking cancer is because it stops the T cells before you have enough to kill all the tumour cells,” he explained.
He came up with the radical notion that if the molecular brakes could be disabled temporarily, it would give T cells a chance to eliminate all the cancer cells. When he tested an antibody against CTLA4 that achieved just that the results were spectacular. Mice with cancer were cured by treatment with the antibodies that inhibit the brake and unlock anti-tumour T-cell activity. “Not only could you treat cancer by ignoring it, but you could do it by not trying to activate anything – you just take the brakes off and let the immune system do what it’s going to do,” he said.
In 2010, an important clinical study showed checkpoint inhibition therapy had striking effects in patients with advanced melanoma. About 20% of people who received the therapy were alive four years after treatment. Such remarkable results had never been seen before in this patient group. The trials led to the therapeutic antibody ipilimumab (Yervoy) being approved for treating late-stage melanoma.

Meanwhile, a similar story was unfolding in Japan. In 1992, Honjo discovered another molecule that influences T cell activity called PD-1 and after years of meticulous experiments in his laboratory at Kyoto University, was able to show that it serves as another braking mechanism in the immune system. Blocking this brake also triggered attacks on cancer cells, but PD-1 worked in a different way to CTLA-4, paving the way for another new treatment capable of destroying tumours.
Clinical researchers were later able to confirm Honjo’s theories. His form of checkpoint inhibition led to responses in more patients and also worked against additional forms of cancer. “I was immensely pleased to hear about a patient whose large tumour had been completely cured by PD-1 blockade therapy, and to watch her enjoying a round of golf on a TV programme about the breakthrough drug,” Honjo said of a woman who received the checkpoint inhibitors to combat ovarian cancer.

By the mid-2010s, both scientists’ checkpoint inhibitors were approved by the FDA and were able to be used to help cancer patients. In 2013, Science magazine selected cancer immunotherapy as the number one scientific breakthrough of the year.
It has since been found that Honjo and Allison’s checkpoint inhibitors have especially strong effects when used together. In 2017, the anti-PD-1 pembrolizumab, became the first cancer treatment of any type to be approved by the FDA for use regardless of where a tumour is located after 40% of patients with 15 different types of tumour responded to the drug.
One of the most striking differences between immunotherapy and other cancer treatments is that it offers patients the potential of permanent protection against a cancer taking hold again thanks to the ability of memory T cells to “remember” the cancer’s identity long after the disease has been eliminated. If cancer cells hide from the immune system and later grow into a tumour, causing a patient to relapse, memory T cells can quickly transform into T cells that can launch an immune response against cancer.
Because of this, Allison has described immunotherapy as more than a cancer therapy. “This is a way of liberating people from a burden of always having every day to be thinking about the fact that you’ve got this disease that can come back and kill you,” he said.
A lasting impact and promising future
The number and range of patients benefiting from immunotherapy is growing, but it does not work for everyone yet and there are side effects including the risk of inducing autoimmunity when the immune system attacks healthy tissues in your body. Honjo hopes that biomarkers will predict suitable candidates for the treatment, while more research will boost the efficacy of checkpoint inhibitors. “We need the power of many, many people to push this therapy in a really satisfactory level,” he said.
The advent of immunotherapy has been described as the cancer equivalent of penicillin, which gave rise to a whole generation of antibiotics that changed medicine, and consigned most previously fatal infections to history.
Both laureates believe that the development of their work so far is only just the beginning. “I hope this therapy will be widely used and reach to almost everybody in the world hopefully by the end of the century just like the infectious diseases almost eradicated during last century,” Honjo said. “I hope this century will be remembered for the century of cancer treatment.”
By Sarah Griffiths, for Nobelprize.org
First published May 2024
Nobel Prizes and laureates
Six prizes were awarded for achievements that have conferred the greatest benefit to humankind. The 12 laureates' work and discoveries range from proteins' structures and machine learning to fighting for a world free of nuclear weapons.
See them all presented here.
